Access to Diabetes Care in the Time of COVID-19

The theme for this year’s World Diabetes Day (November14)—Access to Diabetes Care—really resonates with me.
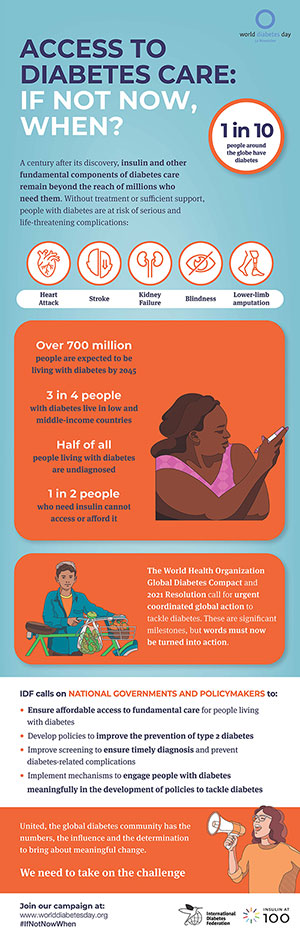
Worldwide, nearly 500 million people have a diabetes diagnosis, and another 232 million people live with undiagnosed diabetes. Without action, this could increase by 51 percent—to 700 million people—by 2045.
Data shows that three out of four people with diabetes live in low and middle-income countries. There are gaps in diagnosing the disease and gaps in access to appropriate care and treatment. Many have lacked needed health care and treatment for diabetes in their country of origin. As people emigrate to the United States, it is important that we offer care to individuals in need.
 What is diabetes?
What is diabetes?
Diabetes is a persistent or chronic condition that occurs when the body’s ability to produce the hormone insulin in the pancreas is impaired, resulting in abnormal metabolism of carbohydrates and elevated levels of glucose in the blood and urine. High blood sugar levels cause serious health impacts, including heart disease, kidney disease, and eye disease.
Diabetic retinopathy is one type of eye disease and an important cause of blindness. It occurs because of long-term accumulated damage to small blood vessels in the retina (back of the eye). Diabetes is the cause of 2.6 percent of blindness globally.
How can COVID-19 bring about high blood sugar?
Throughout the pandemic, you may have heard that people living with diabetes have a greater chance of developing and experiencing serious side effects. Why? Because viral infections can increase inflammation—a strong internal response to an infection or injury—in people with diabetes. This inflammation could contribute to more severe complications, particularly with people who have above-normal blood sugar levels or diabetes that is not well controlled. Having an underlying condition like diabetes and then developing another infection like COVID-19 makes it harder for your body to fight the infection.
In some cases, a person may have undiagnosed diabetes. In some cases, a person might have pre-diabetes, and acute inflammation and/or steroid treatment can push them into having very high blood sugars. An acute stressor can increase insulin resistance enough that a relative deficiency of insulin production is revealed, and glucose goes above the normal level.
A person may have been genetically at risk and have mild stressors (such as being overweight but not necessarily obese) and may be mildly but not completely sedentary. The combination of insulin resistance from the acute infection and high-dose steroids used to treat COVID-19 can cause a significant increase in production of insulin to keep glucose normal but the pancreas may not be able to increase output to that level.
What is known in the scenarios above is that most patients still have “prediabetes” six months later and will likely progress to a Type 2 diabetes diagnosis within five years. In addition, most if not all will be formally diagnosed with diabetes in their lifetime.
If you have had COVID-19, know the warning signs that you might have developed diabetes:
- Frequent urination, which may include waking up at night to urinate and/or increased frequency during the day.
- Increased thirst with blurry vision.
- Inability to regain the weight lost while acutely ill.
- Slow wound healing.
- Fatigue—this one is tough because most people with COVID have fatigue for a prolonged period after the acute illness.
What can you do to prevent diabetes after COVID-19? Focus on losing 15 pounds. Based on the data from populations with prediabetes, we know this can significantly slow the progression to Type 2 diabetes. Losing more weight can also help, but those first 15 pounds are the most important.
We’ve come a long way
Despite the numbers and data, let’s not forget that we have come a long way. In fact, it is 100 years since the discovery of insulin. On July 27, 1921, Canadian surgeon Frederick Banting and medical student Charles Best successfully isolated the hormone insulin to treat diabetes. It marked one of the most important breakthroughs in the history of diabetic treatment.
In January 1922, the first successful insulin injection was provided to a 14-year-old person with juvenile diabetes. This was life-changing for people who suffered from a disease that had previously been considered fatal.
Other milestones include the first specialized insulin syringe (1924), first disposable glass syringe (1954), first blood glucose meter (1974), first human insulin developed (1982), first insulin pen (1985), first islet cell transplantation conducted (2000), and first artificial pancreas developed (2013).
Though we’ve come a long way, medications along with essential services and care are needed to treat diabetes so that serious complications and consequences can be avoided or delayed. Healthy self-care practices can help you avoid or manage your diabetes—eat a healthy diet, get regular physical activity, and maintain stable blood sugar levels.
 Contributor Mary Pat O’Leary, RN, BSN is a senior planner at Aging and Disability Services. She extends appreciation to Dr. Katherine Bennett for assisting with this article and her leadership in training new geriatricians, and thanks all the health care professionals who support and provide quality and compassionate care to those living with diabetes.
Contributor Mary Pat O’Leary, RN, BSN is a senior planner at Aging and Disability Services. She extends appreciation to Dr. Katherine Bennett for assisting with this article and her leadership in training new geriatricians, and thanks all the health care professionals who support and provide quality and compassionate care to those living with diabetes.
More Information About Diabetes and COVID-19
- Diabetes (National Institute of Diabetes and Digestive and Kidney Diseases)
- How COVID-19 Can Lead to Diabetes (NIH Director’s Blog)
- Lifestyle Change Program Details (Centers for Disease Control and Prevention)
- Managing Diabetes (Centers for Disease Control and Prevention)
- Why are people developing diabetes after having COVID-19? (Wexner Medical Center, The Ohio State University)
![AgeWise King County [logo]](https://www.agewisekingcounty.org/wp-content/themes/agewisekingcounty/images/logo.png)